-
Individualized Medicine
Research suggests genetics are key in treating night sweats
Article by Heather Carlson
 Women going through menopause know all too well the discomfort associated with night sweats.
Women going through menopause know all too well the discomfort associated with night sweats.
Hormone therapy is often used to prevent night sweats. But finding the right dose of estrogen can be tricky, with some women needing more estrogen than others to get relief. Why the difference in how women respond to hormone therapy? The answer may be found in a woman’s genes.
A new Mayo Clinic study published in Menopause: The Journal of the North American Menopause Society found that genetic differences appear to play a role in the effectiveness of hormonal treatment for menopausal women.

“In this study, we explored how a genetic variant in a gene that regulates how estrogen is cleared from the blood alters estrogen levels and relief of night sweats in menopausal women. We hope that this study will generate interest in the potential use of genetics to individualize hormone therapy dosage and formulation,” says Ann Moyer, M.D., Ph.D., co-director of the Mayo Clinic Personalized Genomics Laboratory.
The four-year study involved 100 women enrolled in Mayo Clinic’s Kronos Early Estrogen Prevention Study. As part of the study, 33 women were given oral estrogen, 33 received an estrogen patch and the remainder was given a placebo pill or patch. At the time of enrollment, the age of women ranged from 42 to 58 and they were on average 1.4 years past menopause.
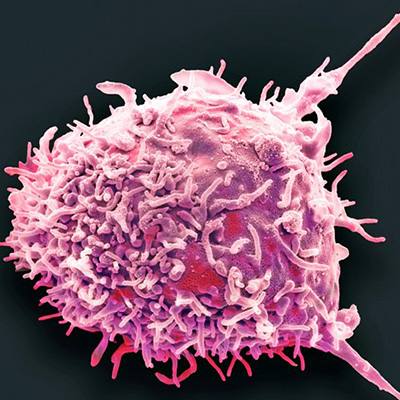
Researchers zeroed in on one specific gene — SLCO1B1. That gene provides instructions for making a protein found in liver cells. That protein transports estrogen from the blood into the liver so that it can be broken down and cleared from the body.
The study showed a significant association between differences in the SLCO1B1 gene and the amount of estrogen in a woman’s system. Genetic differences also helped determine how well a woman responded to hormone therapy. For example, women given an estrogen patch who have a genetic variation that leads to a decreased movement of estrogen from the blood into the liver saw a significantly greater drop in night sweats compared to other women.

“In this study, researchers have demonstrated that pharmacogenomics— differences in the DNA sequences in a woman’s genome — can influence the ability of her body to clear estrogen when it is used to treat her for menopausal symptoms, raising the possibility of more highly individualized dosing of estrogen in that setting,” says Richard Weinshilboum, M.D., co-director of the Mayo Clinic Center for Individualized Medicine Pharmacogenomics Program and a co-author of the study. Pharmacogenomics is the study of how your genes affect the way your body processes and responds to medications.
The hope is that one day, physicians can use a woman’s genetic information to determine the right amount of hormone therapy needed to treat night sweats and other menopause-related conditions, according to Virginia Miller, Ph.D., director of the Mayo Clinic Women’s Health Research Center and the study’s senior author.

“What we would ultimately like to be able to do is get the genetic profile for women so if they are experiencing these conditions of menopause, we can better target the treatment,” says Dr. Miller.
###
Related Resources
Join the conversation
For more information on the Mayo Clinic Center for Individualized Medicine, visit our blog, Facebook, LinkedIn or Twitter at @MayoClinicCIM.
Register to attend this year’s Individualizing Medicine Conference. It will be held in Rochester, Minnesota, on Sept. 12-13, 2018.

Related Articles