-
Biotherapeutics
Platelet-rich plasma: A regenerative approach to healing chronic wounds
By Madelyn Fell
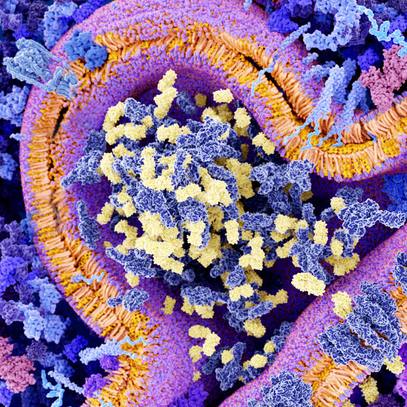
Platelet-rich plasma is the fraction of blood plasma that contains concentrations of platelets that are higher than baseline. Platelet-rich plasma attracts significant interest in the medical and research community since platelets possess various growth factors and cell parts that are critical for tissue repair and regeneration.
Autologous platelet-rich plasma therapy uses injections of a patient's own platelets to accelerate the healing of injured tendons, ligaments, muscles and joints. In this way, platelet-rich plasma injections use patients' own healing system to address and improve musculoskeletal problems.
Mayo Clinic uses platelet-rich plasma to treat osteoarthritis of the knee; forms of tendinopathy, including tennis elbow and plantar fascitis; and as an adjunct therapy in orthopedic surgeries to help patients heal faster after surgical procedures.
Wenchun Qu, M.D., Ph.D., is the director of Regenerative Pain Medicine at Mayo Clinic's Center for Regenerative Medicine. Dr. Qu and his team have explored platelet-rich plasma's implications for wound care.
"Platelet-rich plasma is very safe because it is your own blood product, and it is an effective intervention for chronic nonhealing wounds," says Dr. Qu.
Chronic wounds are among the common chronic medical conditions that significantly affect the elderly population. Chronic wounds affect nearly 15% of Medicare beneficiaries and create a health care burden of $28 to $96 billion per year in the U.S.
The research
In a recently published paper in Mayo Clinic Proceedings, Dr. Qu reports findings from a meta-analysis that evaluates the effectiveness and safety of autologous platelet-rich plasma for wound care. A meta-analysis is an examination of data from numerous independent studies on the same subject to determine overall trends.
This meta-analysis included 20 randomized control trials and five observational studies on 1,952 patients. The studies focused on adults with lower-extremity diabetic ulcers, lower-extremity venous ulcers, and pressure ulcers. Each study compared platelet-rich plasma therapy to other wound care protocols without platelet-rich plasma. In lower-extremity diabetic ulcers, platelet-rich plasma intervention increased the chance of complete wound closure, sped up wound closure, and reduced wound size, compared to management without platelet-rich plasma.
Significance for wound care
Findings of the meta-analysis have significant implications for treatment of lower-extremity diabetic ulcers. An optimal outcome of wound care is to achieve complete wound closure that reduces the risk of infection; tissue necrosis; and osteomyelitis, or bone infections ― all of which are complications known to increase the risk of lower-extremity amputation.

Diabetes can result in deterioration of nerves and blood vessels in extremities. Wounds can sometimes lead to the development of neurotropic ulcers.
Complete healing is difficult to accomplish in most patients with standard care. However, platelet-rich plasma is valuable because it helps accomplish this important goal.
Another highly important factor central to wound care is healing speed. Chronic wounds heal slowly. The longer the healing takes, the higher risk the patient is exposed to infection. Comparison of healing time between platelet-rich plasma and the control group was examined in four studies, of which three reported statistically significant healing time reduction and one showed no difference.
The meta-analysis found that platelet-rich plasma does not cause harm for any of the three wound types studied ― lower-extremity diabetic ulcers, lower-extremity venous ulcers, and pressure ulcers.
Platelet-rich plasma is an effective procedure for chronic lower-extremity diabetic ulcers.

Platelet-rich plasma possesses various growth factors and cell parts that are critical for tissue repair and regeneration.
"The evidence from this decadelong effort studying the risk and benefit of platelet-rich plasma for wound care has concluded that platelet-rich plasma is safe and effective for diabetic wound care. I am glad the evidence provided by this meta-analysis will be used to help improve patients' access to this therapy," says Dr. Qu.
Next steps
Dr. Qu's team will continue to monitor the safety and effectiveness of platelet-rich plasma therapy for chronic diabetic ulcers, and update the public and medical community of their findings. Chronic nonhealing wounds are still a challenging condition that requires more in-depth research for therapies that address repair and regeneration processes. Dr. Qu says future studies will include engineered cell and cell product therapies.
"The goal is to precisely target the gene and molecular processes, and provide a solution specific for each type of chronic wound and each individual patient," says Dr. Qu.
This project was funded by the Agency for Healthcare Research and Quality, Department of Health and Human Services through Mayo Clinic’s Evidence-based Practice Center, which is a major initiative of the Knowledge Synthesis Program in the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
###